September is the PCOS (Polycystic Ovarian Syndrome) awareness month, so I’d like to wave
goodbye to September by shedding some further light on the syndrome and sharing
with our readers some information that might help ladies reach an early
diagnosis as well as some skin related management tips for this difficult
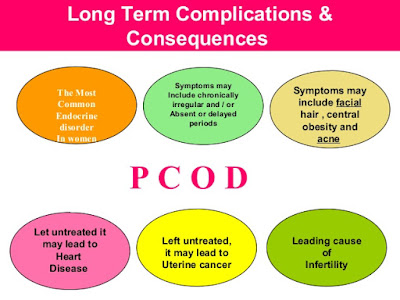
multisystem disease. It’s a grim fact that worldwide PCOS affects 6% to 10% of
women, making it the most common endocrinopathy in women of childbearing age.
Early
diagnosis and establishing a good management plan are key to managing cosmetic
issues and preventing long term health consequences, as there is no cure for
PCOS.
PCOS At A Glance
Common
symptoms of PCOS include irregular or no menstrual periods, acne,
obesity/weight gain/inability to lose weight, breathing problems while sleeping,
depression, oily skin/acne, infertility, skin discolorations, high cholesterol
levels, elevated blood pressure, excessive/abnormal hair growth and
distribution, pain in the lower abdomen and pelvis, multiple ovarian cysts, and
skin tags. Some women have only a few symptoms, while others have several.
How Do You Know If You Have
PCOS?
You
can be diagnosed with PCOS if you have at least 2 of the following 3 criteria
1.
Irregular or absent periods,
2.
Blood tests or physical signs that show high androgens,
3.
Polycystic ovaries.
Health Risks With PCOS
Women
with PCOS have greater chances of developing several serious health conditions,
including life-threatening diseases. Recent studies found that:
·
More than 50 percent of women with PCOS will have diabetes or
pre-diabetes (impaired glucose tolerance) before the age of 40.
·
The risk of heart attack is 4 to 7 times higher in women with PCOS than
women of the same age without PCOS.
·
Women with PCOS are at greater risk of having high blood pressure.
·
Women with PCOS have high levels of LDL (bad) cholesterol and low
levels of HDL (good) cholesterol.
·
Women with PCOS can develop sleep apnea. This is when breathing stops
for short periods of time during sleep.
·
Women with PCOS may also develop anxiety and depression. It is
important to talk to your doctor about treatment for these mental health
conditions.
·
Women with PCOS are also at risk for endometrial cancer. Irregular
menstrual periods and the lack of ovulation cause women to produce the hormone
estrogen, but not the hormone progesterone. Progesterone causes the endometrium
(lining of the womb) to shed each month as a menstrual period. Without
progesterone, the endometrium becomes thick, which can cause heavy or irregular
bleeding. Over time, this can lead to endometrial hyperplasia, when the lining
grows too much, and cancer.
Skin & PCOS
Being
a dermatologist I’d like to focus on the skin-related symptoms of PCOS, which include
oily skin, adult acne, increased/abnormal hair growth, skin tags, and dark
velvety skin patches on neck known as acanthosis nigricans.
Acne and oily skin:
One
of the earliest signs of PCOS is acne and oily skin which are primarily the
result of hormonal disorders caused by androgens (male hormones). PCOS-related
acne tends to flare in areas that are usually considered “hormonally
sensitive,” especially the lower third of the face. This includes your cheeks,
jawline, chin, and upper neck. Ladies with PCOS tend to get acne that involves
more tender knots under the skin, rather than fine surface bumps, and these
acne lesions tend to flare before the menstrual period. This type of cystic
acne doesn’t resolve quickly and takes time to go away.
Unwanted Hair Growth:
Unwanted
hair growth is also triggered by an excess of male hormones leading to
excessive growth of facial hair, as well as hair on the abdomen and around the
nipples. The same hormones are also responsible for hair loss on scalp, which
is why ladies suffering with PCOS struggle with thinning hair on scalp and
increased hair on face and body at the same time. Shaving, waxing,
depilatories, and tweezing are all options, but each has its limitations and
each demands ongoing efforts. Vaniqa cream has shown promising results to
reduce facial hair growth. Laser hair reduction is another good long-term
option.
Medications
called anti-androgens may reduce hair growth and clear acne. Spironolactone
(Aldactone), first used to treat high blood pressure, has been shown to reduce
the impact of male hormones on hair growth in women. Finasteride (Propecia), a
medicine taken by men for hair loss, has the same effect. Anti-androgens are
often combined with birth control pills.
These medications should not be taken if you are trying to become
pregnant.
Metformin
(Glucophage) reduces insulin levels, and this change, in turn, reduces the
ovarian testosterone levels by competitive inhibition of the ovarian insulin
receptors. This drug is effective in treating increased hair in women with
PCOS.
Hair Loss:
The
type of hair loss women with PCOS experience is directly related to the excess
production of male hormones caused by the disorder. Referred to as male-pattern
baldness, it can be successfully treated with over-the-counter medications
containing Minoxidil or Saw Palmetto along with oral contraceptive pills (Diane 35) and anti-androgen (Spironolactone) medication.
Skin Darkening:
The
brown skin discolorations that occur with PCOS are unique, and are called
“Acanthosis Nigricans”. They appear as darkened, velvety swaths of dark brown patches
that most often develop on the nape of neck, armpits, inner thighs, or under the
breast areas. Although these discolorations are not related to sun damage, the
treatment is the same: daily exfoliation, sunscreen, and use of a topical
over-the-counter skin-care product with 2% hydroquinone or other skin
lightening agents. For stubborn cases, you may need a prescription-strength
skin lightener that contains 4% hydroquinone.
Skin Tags:
Fleshy
skin growths in the armpits and neck regions are commonly spotted in PCOD. Once
the hormones are fixed we can surgical remove or cauterize these growths.
Management Plan
Lifestyle
modifications are considered first-line treatment for women with PCOS. Such
changes include the following:
·
Diet - Low-fat, high-carbohydrate
diets may increase insulin levels, so you may want to consider a
low-carbohydrate diet if you have PCOS. Don't severely restrict carbohydrates;
instead, choose complex carbohydrates, which are high in fiber. The more fiber
in a food, the more slowly it's digested and the more slowly your blood sugar
levels rise. High-fiber carbohydrates include whole-grain breads and cereals,
whole-wheat pasta, bulgur wheat, barley, brown rice, and beans. Limit less
healthy, simple carbohydrates such as soda, excess fruit juice, cake, candy,
ice cream, pies, cookies and doughnuts.
·
Exercise - Exercise helps lower
blood sugar levels. If you have PCOS, increasing your daily activity and
participating in a regular exercise program may treat or even prevent insulin
resistance and help you keep your weight under control.
·
Weight loss - Obesity makes insulin
resistance worse. Weight loss can reduce both insulin and androgen levels and
may restore ovulation. No single specific dietary approach is best, but losing
weight by reducing how many calories you consume each day may help with
polycystic ovary syndrome, especially if you're overweight or obese. Use
smaller plates, reduce portion sizes and resist the urge for seconds to help
with weight loss. Ask your doctor to recommend a weight-control program, and
meet regularly with a dietitian for help in reaching weight-loss goals.
Medications used in the management of
PCOS include the following:
·
Oral contraceptive agents (eg, ethinyl estradiol, medroxyprogesterone)
·
Antiandrogens (eg, spironolactone, leuprolide, finasteride)
·
Hypoglycemic agents (eg, metformin, insulin)
·
Selective estrogen receptor modulators (eg, clomiphene citrate)
·
Topical hair-removal agents (eg, eflornithine)
·
Topical acne agents (eg, benzoyl peroxide, tretinoin topical cream
(0.02–0.1%)/gel (0.01–0.1%)/solution (0.05%), adapalene topical cream
(0.1%)/gel (0.1%, 0.3%)/solution (0.1%), erythromycin topical 2%, clindamycin
topical 1%, sodium sulfacetamide topical 10%)
The
optimal management for PCOS is a multi-factorial approach involving diet and
lifestyle modification along with appropriate medication. If you think that you
have any symptoms which point towards PCOS speak to your GP as soon as possible.






Dr itua herbal medicine is mighty and genuine,I use to use Melissa oil and Lavender Healing herbs but result were just still the same.But using Doctor Itua herbal medicine cured my herpes & Hepatitis C final and I have being living for 3 years now No Sores.My herpes is truly gone.Contact him if you interested of his herbal medicine too Dr itua can as well cure the following....HIV...HERPES,,,,HEPATITIS,CANCER,Neuro-infectious Disease,Neuromuscular Diseases,Diabetes,Depression,Anxiety,Hemorrhoid,Yeast infection,Lupus,Shingles,Psoriasis,Back Pain,ALS, Get ex back, Tinnitus.drituaherbalcenter@gmail.com Or Website www.drituaherbalcenter.com
ReplyDelete